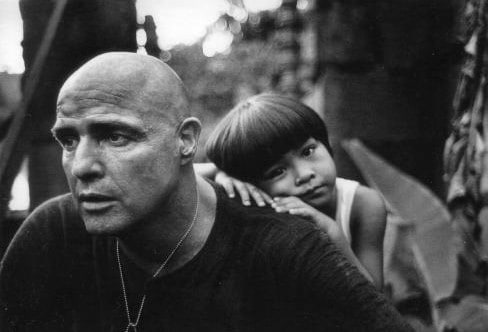
Many U.S. military veterans, returning from long tours of duty overseas, many of those in far-off, hostile environments, are coming back with a range of serious mental health disorders, such as post-traumatic stress disorder (PTSD) and depression, with tendencies to suicidal ideation, and suffering from substance use disorders (SUDs), where they resorted to self-medicating, either to simply cope with their circumstances or to deal with chronic pain sustained during their service. In a perfect world, their first port-of-call should be a drug and alcohol rehab for veterans.The character of Colonel Walter E. Kurtz, played by Marlon Brando, in the 1979 Francis Ford Coppola film “Apocalypse Now” was one of the first significant instances highlighted by Hollywood of the devastating mental impact that the U.S. military has endured as part of their active service, whether it’s the Second World War, Korea, Vietnam, Iraq, Afghanistan or elsewhere that their duty has been called upon.
You have to have men who are moral, and at the same time who are able to utilize their primordial instincts to kill without feeling, without passion, without judgment… without judgment. Because it’s judgment that defeats us.” – Colonel Walter E. Kurtz, from the 1979 Francis Ford Coppola film “Apocalypse Now”
However, the U.S. public in general was already used to the sight of homeless Vietnam veterans sleeping on street corners, many drug addicts or alcoholics or both, and many with untreated mental health disorders and behavioral problems. Later, it would be military personnel returning from Iraq & Afghanistan who would take their place on those same street corners, in drug dens and darkened bars, and in the nation’s prisons.However, such problems with returning servicemen and women had been publicly acknowledged previously. The famous term “thousand-yard stare” or “two thousand-yard stare,” used to define the glazed, blank and disassociated look of soldiers emotionally detached from the horrors around them, was first popularized back in 1945, towards the end of Second World War, by artist and war correspondent Tom Lea, who entitled one painting as “Marines Call It That 2,000 Yard Stare,” and published by Life Magazine.Today, we would medically define the thousand-yard stare of WW2 as either a precursor or a symptom of PTSD. It’s the year 2020, and that thousand-yard stare can still be seen in the eyes of returning U.S. veterans.
Returning U.S. Veterans: Damaged & Broken
According to the National Conference of State Legislatures, there are 18.8 million U.S. veterans now living back home, making up 7.6% of the national population. Out of this high number, around half are enrolled in the U.S. Department of Veterans Affairs Health Care Program.Furthermore, a significant percentage of returning military personnel have a range of diagnosed and, worryingly, undiagnosed health conditions, such as injury, trauma-related health issues, such as military sexual trauma (MST), and mental health disorders, like PTSD, which, in turn, can lead to suicide and suicidal ideation, and SUDs, including alcohol use disorder (AUD) and opioid use disorder (OUD), caused by abusing opioid pain management after an injury has been sustained.Looking at each of the most harmful and dangerous health conditions, in turn, the statistics provided within this article, when viewed as a whole, present a disturbing image of physically and mentally damaged military servicemen and women returning to a nation that could and should do more to treat, counsel, medicate and assist those who have suffered in the line of duty and in their service to the U.S.
U.S. Veterans’ Mental Health: Focus on Washington State
Periodically, the VA publishes data, by U.S. state, of veteran suicide rates. The latest, which was published in 2017, shows from the data for Washington state, accounting for age differences, that the WA veteran suicide rate:
- Was not significantly different from the national veteran suicide rate, but
- Was significantly higher than the national suicide rate (31.3%, compared to 18.1%)
Furthermore:
- There were 176 WA veteran suicides in 2017 (164 men and 12 women)
- The WA veteran suicide rate was 31.3%, whereas the WA general population suicide rate was only 21.9%, and
- The highest veteran suicide rate was found in the 18-34 age group – 46.4% (nearly half)
The Challenges Facing U.S. Veterans: Health Care Access & Readjustment to Civilian Life
Many U.S. military personnel returning from overseas tours will come back with one of the common conditions described above, and some return suffering more than one, known as comorbidity. Examples of comorbid conditions include physical issues such as TBI and chronic pain. Those suffering from substance addiction (SUD or AUD) and a mental health disorder, such as depression, is another example of comorbidity and is specifically known as a co-occurring disorder or dual diagnosis. In medicine, there is a specific comorbid condition known as polytrauma clinical triad (PCT) – the presence of TBI, PTSD, and chronic pain, which has been linked to an increase in the risk of suicidal behavior.U.S. Veterans Affairs (VA), although present in some form even in 1776, way back to the American Revolutionary war, was created in its current form in 1930, when the U.S. government began to offer consolidated and structured services to its veterans. One of the most important parts of these services was the provision of health care benefits for the treatment of personnel with service-related physical or mental injuries and overseen by the Veterans Health Administration (VHA).Although the health care provided is as good as or better than that provided by private or non-VHA public practices, access and quality still varies widely across the system. Several notable studies have shown that:
- Many veterans don’t receive any treatment following PTSD, SUD or depression diagnoses
- Many veterans don’t know how to apply for veterans’ mental health care benefits
- Many veterans are unsure if they are eligible, and even
- Many veterans are unaware that mental health care benefits are actually available to them
Other reported barriers to VHA health care services include:
- Difficulty getting to medical facilities provided, eg. inconvenient location, a lack of transportation, etc
- Concerns about taking time off work, and
- Fear of discrimination, primarily due to the stigma around mental health issues, leading to a loss of custody or contact with their children, or a loss of medical or disability benefits
In terms of readjusting to civilian life after their military service ends, U.S. veterans also have to face and overcome social and economic challenges, such as finding employment after deployment – not such an easy task with the hit the economy has taken with the COVID-19 pandemic, eg. high rates of unemployment (rates not seen since the financial crisis of 2007-2008). Unfortunately, this type of military readjustment data is not available.
The Link Between Homelessness, Mental Health Disorders & Substance Addiction for U.S. Veterans
The “2014 Annual Homeless Assessment Report (AHAR) to Congress” report, published by the U.S. dept. Of Housing & Urban Development, reported that on a single night in January 2014, there were approximately 50,000 homeless veterans in the U.S. Furthermore:
- Male veterans are 1.3 times more likely to become homeless than non-veteran men
- Female veterans are 3.6 times more likely to become homeless than non-veteran women
- 70% of homeless veterans suffer from a substance use disorder
- 45% of homeless veterans suffer from mental illness, predominantly PTSD
Here in Washington state, the city of Seattle is being particularly badly affected by homelessness, addiction rates, and spiraling crime. At the last count, there were 12,000 homeless in the city, and a significant number of these are military veterans.
1. U.S. Veterans with Trauma
Military conflict, harsh environments, and heightened stress are all precursors to severe reactions to traumatic events. Many returning veterans have seen and experienced things that would be the stuff of nightmares for the likes of us ordinary civilians. However, it’s not just external factors that can instigate a traumatic event – sometimes, the traumatic event happens within the confines of the military compound. It is important to remember that untreated trauma can lead to severe and profound effects on daily life and normal function.In general terms, trauma can be defined as a condition resulting “from an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or threatening and that has lasting adverse effects on the individual’s functioning and physical, social, emotional, or spiritual well-being.”Imagine sharing the lives of your comrades and friends, eating, sleeping and training together 24/7, sharing the fear and exhilaration of combat, only to watch as their lives are brought to an abrupt end by a roadside IED, an unseen sniper’s bullet or a missile fired from a distant unreachable location. No U.S. veteran is immune to the devastating effects it brings.
Military Sexual Trauma (MST)
Sometimes, the enemy is the enemy within… “Military sexual trauma” (MST) is the term used to describe a sexual assault or harassment experienced during military service. Obviously, servicewomen are more at risk of MST in such a male-dominated environment; however, MST is any sexual activity that any military person, male or female, is involved in – against their will, and without their consent.Examples of MST include:
- Rape – physically forced to have sex
- Pressured or coerced into sexual activities, eg. threats of retaliation/harm
- Sexual contact without consent, eg. when the victim is asleep or intoxicated
- Sexual touching
- Comments about the body or sexual activities
- Unwanted or threatening sexual advances
Like other kinds of experienced trauma, MST can negatively affect a person’s mental and physical wellbeing. If left untreated, these negative effects will continue for years. These negative effects include:
- Depression/anxiety
- Substance addiction
- Disturbed sleep
- Feeling isolated
- Anger management problems, and
- Physical health problems
It is estimated that 25% of female veterans and 1% of male veterans have experienced MST. Accurate statistics are unlikely because of the undeserved stigma attached to such trauma.
The Impact of Deployment on U.S. Military Families
It is important to acknowledge that it is not just the serving family member that is at risk of all the issues described here. Common mental challenges experienced by both service members and their families include:
- Fears for the safety of the service member
- Anxiety over deployment-related challenges and responsibilities, and the wellbeing of the children involved; in fact, one-third of children with at least one deployed parent experience depression, anxiety and/or behavioral disorders
The 2012 “Army Gold Book,” a periodical report that assesses the challenges experienced by soldiers and their families, reported:
- 56% of spouses experienced stress in 2010
- Nearly half (44%) of the spouses reported concerns about finances
- Two-thirds reported that they had less than $500 in savings, and
- 19% of spouses reported they were in counseling, primarily for stress, family and/or marital issues
2. U.S. Veterans with Traumatic Brain Injury (TBI) & Polytrauma
Traumatic Brain Injury (TBI)
With the rise in the use of improvised explosive devices (IEDs) in military conflicts, the number of cases of traumatic brain injury (TBI) have risen significantly over recent years. TBI is medically defined as “a traumatically induced structural injury of the brain or physiologic disruption of normal brain function resulting from an external force”, typically caused by a blow or jolt to the head (or, the worst case scenario – an object penetrating the brain). It can result in changes in consciousness, disorientation, confusion, memory loss, and the potential to slip into a coma. However, not all head injuries can result in a TBI.Possible causes of TBI include:
- Head being hit with a fist or object, eg. piece of wood
- Head hitting an object, eg. car dashboard in an accident, or by falling to the ground
- Head affected by nearby blast or explosion
The severity of the injury depends on:
- Length of time unconscious
- Level of memory loss or disorientation
- Responsiveness after the event
Important: Mild TBI is also known as concussion.TBIs can result in continuing difficulties for the victim, which can include:
- Physical changes
- Behavioral changes, and
- Cognitive issues
- Being prone to:
- Headaches
- Dizziness
- Fatigue
- Irritability
- Concentration issues
TBI Treatment: Usually focusing on the symptoms that cause the most issues with daily function, treatment can include:
- Medication
- Cognitive and behavioral learning strategies
- Rehabilitation:
- Physical therapy
- Occupational therapy
- Speech-language therapy)
- Assistive devices and technologies
Known in military circles as one of the “signature injuries” of recent Iraq and Afghanistan conflicts, the Defense and Veterans Brain Injury Center (DVBIC) reports nearly 350,000 diagnoses of TBI in the U.S. military since 2000. Among those deployed, estimated rates of probable TBI range from 11-23%.
Polytrauma
Polytrauma occurs when a person experiences injuries to multiple body parts and organ systems, often, but not always, as a result of blast-related events. TBI frequently occurs in polytrauma in combination with other conditions, such as:
- Amputation
- Burns
- Spinal cord injury (SCI)
- Auditory and visual damage
- Post-traumatic stress disorder (PTSD)
As mentioned previously, a rising type of polytrauma seen in returning veterans is polytrauma clinical triad (PCT) – the presence of TBI, PTSD, and chronic pain.
3. U.S. Veterans with Mental Health Disorders
Post Traumatic Stress Disorder (PTSD)
Post-Traumatic Stress Disorder (far more commonly known as PTSD) is a type of anxiety disorder that develops after someone has been exposed to a trPost-Traumatic Stress Disorder (far more commonly known as PTSD) is a type of anxiety disorder that develops after someone has been exposed to a traumatic event where they felt either fear for their life or fear of serious physical harm. Traumatic events that can trigger PTSD include:
- Sexual abuse
- Violent personal assaults (a rising issue among all first responders)
- Natural or man-made disasters, or
- Military service
Incidence rates of PTSD vary widely depending on the military conflict and era. However, looking at recent conflicts:
- In one major study of 60,000 Iraq and Afghanistan veterans, 13.5% of deployed and non-deployed veterans were positive for PTSD
- Other studies show the rate to be as high as 20% to 30%
- Around half a million U.S. veterans who served in these wars over the past 13 years have been clinically diagnosed with PTSD
Again known as one of the “signature injuries” of deployments in Iraq and Afghanistan, official military reports state that the prevalence of TBI and PTSD among returning U.S. veterans ranges from 19.5% to 22.8% for the brain injury, and up to 24.4% for the mental health disorder (nearly 1 in 4).Furthermore, 77.3% of active military personnel hospitalized for PTSD had a comorbid mental health diagnosis, and this percentage has actually increased every year from 2006-2012. Additionally, alcohol abuse or AUD was a frequent comorbidity – 27.8% with a dual diagnosis.
Depression
Depression, known medically as major depressive disorder or as clinical depression is a common but serious mood disorder. It causes severe symptoms that constantly affect your feelings and thoughts, and affects all daily activities, such as sleeping, eating, and working. Depression can manifest in U.S. veterans in the following ways:
- Persistent Depressive Disorder (Dysthymia):
- A depressed mood that lasts for at least two years
- Psychotic Depression:
- Severe depression, plus some form of accompanying psychosis, such as having delusions or hallucinations
- Seasonal Affective Disorder (SAD):
- The onset of depression during the winter months, accompanied by social withdrawal, increased sleep, and weight gain
Because many military personnel do not seek treatment for depression, it is estimated that between 14-19% of servicemen and women experience depression after deployment. It should also be noted that TBIs and polytrauma can trigger episodes of depression.
4. U.S. Veterans: Suicide & Suicidal Ideation
Suicide and its ideation (thinking about the act of suicide) has limitless causes.Suicide ideation, thinking about the act, is normally the result of feeling like you are unable to cope with life as it is now. Additionally, there is also a genetic link to suicide – people who commit suicide are far more likely to have such history within their family line.Suicide attempts are more common among men; however, men are far more likely to succeed in their attempt, as they employ more lethal methods, eg. firearms – usually within reach of active military personnel. Those most at risk of suicide or suicide ideation, however, are people who:
- Have attempted suicide previously
- Are severely depressed
- Have experienced a traumatic event
- Suffer from SUD (drugs and/or alcohol)
- Feel suicidal and have access to or own a firearm
- Have an underlying psychiatric disorder, eg. major depression or PTSD
- Have a family history of:
- Mental disorders
- SUDs
- Suicide, or
- Violence, including physical or sexual abuse
- Have chronic disease, chronic pain or terminal illness
- Are LGBTIQ in an unsupportive family/environment
In recent years, suicide and suicidal ideation have become an increasing concern for U.S. veterans and their families. According to a 2014 report by the Department of Defense, there were 1,080 suicide attempts (with 245 suicides) among active-duty service members for all armed services in calendar year 2013.Veterans who screened positive for PTSD were 4 times more likely to report suicidal ideation than veterans who did not, and the likelihood of suicidal ideation was 5.7 times greater in veterans who screened positive for PTSD and two or more comorbid disorders. Studies have consistently shown that veterans’ needs peak several decades after their military service, highlighting the necessity of managing current problems.Lastly, the suicide rate among active-duty U.S. military personnel reached 24.8 per 100,000 people in 2018, significantly higher that the rate of the U.S. general population. The year before, the rate was 21.9 per 100,000 troops. Looking at Pentagon reports from 5 years ago, and the suicide rate among servicemen and women was only 18.5 per 100,000 service members. Clearly, it’s a worsening problem.
5. U.S. Veterans with Substance Use Disorder (SUD) & Dual Diagnosis
In sharp contrast to the huge number of young, heroin-addicted U.S. veterans who returned from the Vietnam War, the military personnel of this generation, returning from Iraq and Afghanistan, are predominantly addicted to or abusing alcohol and prescription opioid painkillers – an actual path to heroin, in fact, for some suffering with opioid use disorder (OUD). Both of these require professional treatment with an accredited drug and alcohol rehab center.If the substance use disorder is combined with the presence of a mental health disorder, like PTSD, and known as dual diagnosis (or co-occurring disorder), both disorders need to be treated simultaneously. Failure to do this will cause the untreated disorder to prompt the return of the other. Again, this requires professional addiction treatment with a recognized drug and alcohol rehab center that offers dual diagnosis treatment.
- Alcohol: Just over one-third of U.S. veterans returning from Iraq and Afghanistan either engaged in hazardous drinking behaviors or met the criteria for AUD. In the Marine Corps, this rate rises to nearly half.
- Opioids: A 2017 study of U.S. veterans with opioid pain management prescriptions found that 75% of these were terminated by the physician because of the misuse of pain relief medication.
As this article has clearly shown, the experiences of military service members can be very stressful and may lead to problematic drug & alcohol use – especially for those who’ve been deployed to combat. The military’s zero-tolerance policies and the high level of stigma attributed to drug & alcohol misuse prevent many from getting the vital help they need.