Do you use drugs or drink too much because you are depressed?Or are you depressed because you have a drug or drinking problem?As it turns out, both answers may be true.
“Get your loved one the help they need. Our substance use disorder program accepts many health insurance plans, this is our residential program.”
What is Depression?
“Every man has his secret sorrows which the world knows not; and often times we call a man cold when he is only sad.” ~ Henry Wadsworth Longfellow Let’s first address what depression ISN’T. Depression is not the same as just being sad. Sadness is a temporary feeling brought on by some difficult or painful event in our lives—we feel sad about something. It is a normal human emotion that we all feel from time to time. Depression, on the other hand, is an abnormal negative emotional state. A depressed person will struggle with overwhelming feelings of not just sadness, but also hopelessness, unimportance, and loss of motivation. And rather than being sad about something specific, that person may be depressed about EVERYTHING. Of special relevance, a person who is merely sad will start to feel better when either something changes or they have adjusted to the situation. Over time, sadness fades. But depression doesn’t require a painful event as a trigger. In fact, many people struggling with depression feel bad even when there is nothing identifiably wrong. As a psychological disorder, the major depressive disorder may negatively affect virtually every area of the person’s life, including their relationships, career, eating habits, ability to sleep, and even their overall physical and mental health. Risk factors for clinical depression include:
- Family history—Up to 40% of the risk is attributable to genetics.
- Childhood trauma
- Chronic pain or health problems
- Certain medications
- Major life changes
- Substance abuse
Depression affects close to 20 million adults in America and 216 million people worldwide.
What to Watch Out For: Symptoms of Depression
“Depression is awful beyond words or sounds or images…it bleeds relationships through suspicion, lack of confidence and self-respect, the inability to enjoy life, to walk or talk or think normally, the exhaustion, the night terrors, the day terrors.”~ Kay Redfield Jamison,An Unquiet Mind: A Memoir of Moods and MadnessTypically, depression symptoms persist more than two weeks and may include:
- Sadness
- Crying jags
- Emotionality
- Irritability
- Easily frustrated
- Angry outbursts
- Emptiness
- Hopelessness
- Helplessness
- Inadequacy
- Low self-esteem
- Poor work or school performance
- Loss of interest in outside activities or hobbies
- Decreased sex drive
- Social withdrawal and isolation
- Sleep disturbances—insomnia OR excessive sleeping
- Constant fatigue
- Lack of energy
- Inability to concentrate
- Slowed thinking and confusion
- Increased anxiety
- Loss of appetite and unhealthy weight loss OR “comfort eating and excessive weight gain”
- Abnormal body movements
- Memory problems
- Overwhelming guilt or shame
- Fixation on the past
- Unexplained physical pain
- Increased use of alcohol and/or drugs
- Suicidal thoughts or attempts
Dual Diagnosis: Addiction and Depression
“The difference between feeling down and being depressed is like the difference between having too much to drink one night and being an alcoholic.”~ Patricia L. Owen, I Can See Tomorrow: A Guide for Living with DepressionAccording to the most recent National Survey on Drug Use and Health, there are 19.7 million Americans age 12 or older who have struggled with some type of SUD within the past year—alcoholism, illicit drug abuse, or the misuse of prescription medications.The NSDUH also reports that 17.3 million US adults have experienced at least one major depressive episode during the past year, as have another 2.3 million youths between the ages of 12 and 17. Of those adults with an MDE, almost 64% suffered severe impairment as a result. And among young people with a past-year MDE, the impairment rate jumps to nearly 71%.Among people with recurring major depression, 18% have a drug use disorder and 16.5% have an alcohol use disorder. Conversely, about 20% of people with SUD have a co-occurring mental disorder such as anxiety or depression.
“We treat both addiction and co-occurring disorders and accept many health insurance plans. Take a look at our inpatient program.”
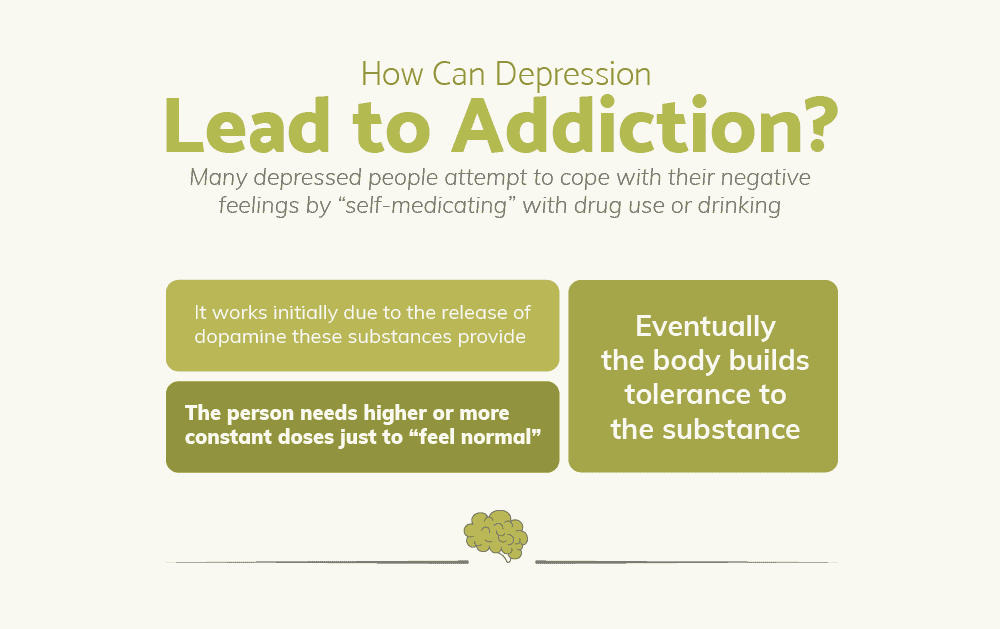
How Can Depression Lead to Substance Abuse and Addiction?
Depression triggers severe emotional pain. Many depressed people desperately attempt to cope with these uncomfortable negative feelings by “self-medicating” with drug use or excessive drinking. At first, these substances offer effective, if extremely temporary, relief from the symptoms of depression.It seems to make a lot of sense in the beginning—having a few drinks or taking a couple of pills, just to feel better and take the edge off. And here’s the thing—alcohol and drugs DO work, at least for a while. They help the person to feel happier and allow them to forget about their pain, fear, and sadness.How do they do this?Every time a person takes a drink or uses an illicit drug, a massive release of dopamine—the neurotransmitter associated with reward, pleasure, learning, memory, and motivation—is triggered.Eventually, however, the person’s dopamine receptors become fatigued from the constant artificial overstimulation. This leads to a diminished response to intoxicants, meaning the person has to consume increasingly-larger amounts to feel the same pleasurable effects.This is known as tolerance.Over time, the brain almost completely stops triggering the release of virtually ANY dopamine unless drugs or alcohol are used. The only time they are able to feel motivation or pleasure—or even function with any degree of normalcy— is when they are drinking or using.This is known as dependence.This is why a severely-dependent person might lose interest in friends, hobbies, once-enjoyed activities, and sometimes, even sex—because they no longer derive any pleasure from these things.According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), tolerance, dependence, and such a loss of interest are among the major symptoms of a diagnosable Substance Use Disorder, the medical condition formerly known as addiction.
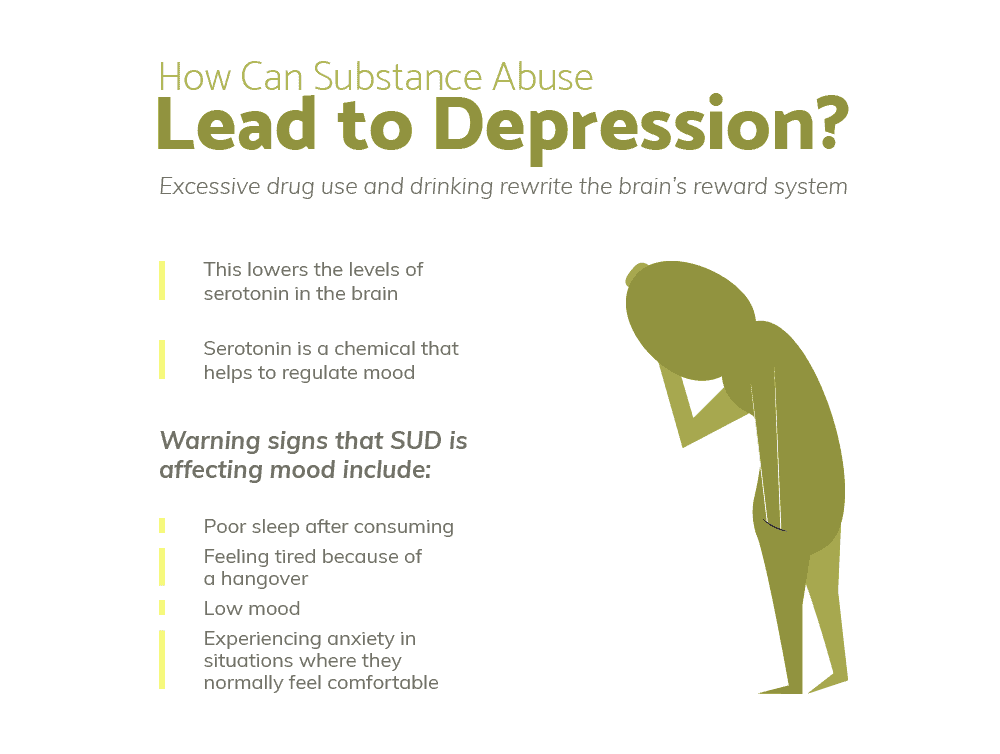
How Can Substance Abuse Lead to Depression?
Over time and with repeated and increasing use, alcohol and drugs eventually contribute to the problem of depression. And while no one becomes an addict intentionally, the tragic transition from recreation or self-medication to compulsion and addiction can happen faster than you might think.This is particularly true for someone who already uses or abuses substances recreationally. Their brain has already been “primed” for addiction. For example:
- According to a study conducted by the University of California, changes to the brain that support alcoholism start with the very first lifetime drink.
- Cocaine permanently alters the brain’s reward pathways after the first use.
And as consumption increases and use worsens to use to abuse and addiction, the consequences also become more serious—relationship problems, health issues, legal entanglements, etc. These new difficulties can cause the person to feel even more anxiety and depression.So, they cope the only way they know how, by self-medicating even more…which of course causes more problems. It becomes a self-perpetuating downward spiral.Of special relevance, continued use despite negative consequences is another primary symptom of SUD.
Booze and the Blues: Alcohol and Depression
“The World Health Organization (WHO) has identified alcohol and depression as the third and fourth largest risk factors for disease burden and leading causes of disability. Co-occurring Alcohol Use Disorder and depression has been linked to a more severe course of illness and worse treatment outcomes.”~ Michael O’Hara and C. Steven Richards, Editors, The Oxford Book of Depression and ComorbidityResearchers have found a possible strong genetic relationship between alcoholism and depression. Comorbidity runs in families. This means that anyone with a family history of either disorder is at far greater risk of developing the other.Regular drinking can result in a condition known as alcohol-induced depression. This is because alcohol is in itself a depressant, and many of its effects mimic the symptoms of depression. A person under the influence of alcohol is also more likely to make poor decisions that can contribute to worsened depression.Additionally, chronic alcohol abuse lowers serotonin levels in the brain. Serotonin is known as the “feel-good: chemical because it is the neurotransmitter responsible for mood regulation. Strangely, while serotonin depletion doesn’t directly cause depression, healthy levels help prevent depressive episodes.
Not Killing the Pain: Opioids and Depression
“Chronic pain and depression go hand in hand. You almost have to assume a person with chronic pain is depressed and begin there…The real pain comes from the losses. Losing a job, losing respect as a functional person, loss of sexual relations, all these make people depressed.”~ Dr. Steven Feinberg, MD, Adjunct Associate Clinical Professor, Stanford University School of Medicine.Sufferingchronic pain has been linked to depression:
- Between one-fourth and over half of the chronic pain patients are depressed.
- 65% of people with depression also experience constant or recurring pain.
- Patients whose independence is limited due to chronic pain are most at-risk for depression.
Also significant, a 2013 study conducted by St. Louis University researchers found that the long-term use of opioids ALSO Increases the risk of new-onset depression. Compared to those patients who received the opioid painkillers for less than 90 days
- Patients given opioid medications for between 90 and 180 days had a 25% greater risk of depression.
- Patients taking opioids for more than 180 days were at a 53% higher risk.
These findings agree with later2016 research that identified a connection between depression and long-term opioid use. Nearly 20% of patients receiving opioids for more than 90 days will exhibit symptoms of major depression.As Dr. Jeffrey Scherer, Ph.D., an Associate Professor of Family and Community Medicine at St. Louis University says, “These findings suggest that the longer one is exposed to opioid analgesics, the greater is their risk of developing depression. Opioids have long been known to allay pain and suffering, but reports of adverse effects are abundant and continue to emerge…Patients and practitioners should be aware that opioid analgesic use of longer than 30 days imposes risk of new-onset depression.”
The Crash: Stimulants and Depression
“Stimulants help to overcome feelings of low energy, fatigue, and low self-esteem, problems associated with depression… When users of cocaine and amphetamines describe the “euphoria” these drugs produce, what they are more likely experiencing is the relief from dysphoria associated with painful depressive reactions and feelings.”~ Mark J. Albanese and Edward T. Khantzian, Understanding Addiction as Self Medication: Finding Hope Behind the PainOn the one hand, the use of stimulants such as cocaine or methamphetamine produces immediate effects that are the opposite of depressive symptoms—confidence, euphoria, and a burst of energy.But following the “up” is always the “down”. When these kinds of drugs wear off, stimulant abusers then experience a crash that leaves them totally drained. The drug-induced energy becomes extreme fatigue, to the point of exhaustion.And because coke and meth severely impair the brain’s reward system, addicts who once experienced a powerful surge of pleasure every time they used may develop a condition known as anhedonia—an inability to take interest or feel pleasure from any other source.These are some of the reasons why 40% of meth users have a lifetime history of major depression. Significantly, the risk rises again among intravenous drug users, compared to those people who snort or smoke meth.
Dark Emotions from Lighting Up: Marijuana and Depression
“We should try to discourage young people from using cannabis, especially those who might be psychologically vulnerable.”~ Dr. Louise Arsenault, Ph.D., King’s CollegeDespite the perception that smoking marijuana may help alleviate depression, there is a large body of evidence suggesting the opposite—that cannabis can, in fact, increase the likelihood of depressive episodes, especially among heavy users and young people. According to various sources:
- Up to 55% of marijuana abusers exhibit symptoms of clinical depression.
- Patients diagnosed with Cannabis Use Disorder are 6.4 times more likely to also receive a diagnosis of co-occurring depression.
- Marijuana use during childhood or adolescence increases the risk of major depression by 17%.
- Among young women, weekly marijuana use doubles the risk of depression.
- Daily marijuana use by young women increases the risk by up to FIVE-FOLD.
- Individuals who have any history of cannabis dependence are three-and-a-half times more likely to suffer major depression.
“We accept many health insurance plans. Get your life back in order, take a look at our residential program.”
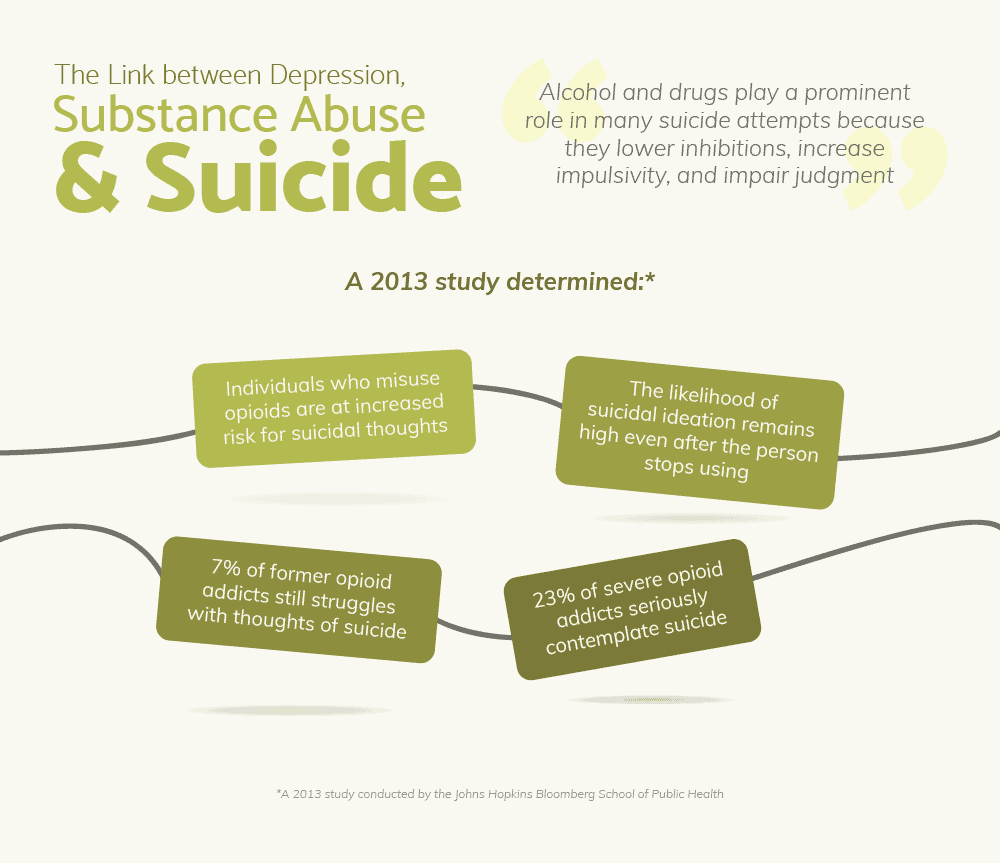
The Link between Depression, Substance Abuse, and Suicide
“If you’re looking for warnings, excessive drinking and drugging is a sign larger than the old Canadian Club Whiskey billboard in Times Square. The last stage of alcoholism before the alcoholic either dies or gets sober is a sense of hopelessness. Isn’t hopelessness a synonym for depression?” ~ Jamie Brickhouse, author of Dangerous When Wet: A Memoir There is a disturbing trend in the United States. The Centers for Disease Control and Prevention reports that the suicide rate has climbed 28% in less than 20 years. To put that in perspective, there are just three causes of death that are going up – drug poisonings, suicides, and Alzheimer’s disease. And two of those three are listed among the primary reasons why life expectancy in America went down in 2017.
- Mental disorders – such as depression – are the #1 cause of suicide.
- Roughly 90% of completed suicides are by individuals with a mental illness.
- Substance abuse is the #2 cause.
- Compared to the general population, people who abuse alcohol or drugs have a risk of suicide that is oversix times higher.
- 60% of victims are intoxicated at the time of their suicide.
- Alcohol abuse is the most accurate predictor of a future suicide attempt.
- In fact, alcoholics have a suicide risk that is five times higher than people who do not abuse alcohol.
- 30% of suicide victims have some degree of Alcohol Use Disorder.
- 2 out of every 3 suicide victims were drinking prior to taking their lives.
- Nearly 9 in 10 alcohol-dependents/addicted suicide victims have a personal history of mental illness.
Alcohol and drugs play a prominent role in so many suicide attempts because they lower inhibitions, increase impulsivity, and impair judgment. In 2013, a study conducted by the Johns Hopkins Bloomberg School of Public Health found that individuals who misuse opioids such as heroin or prescription painkillers are at increased risk for suicidal thoughts. Of special relevance, the research also determined that the likelihood of suicidal ideation remains high even after the person stops using drugs. 7% of former opioid addicts who had not used in more than a year still struggled with thoughts of suicide. This rate is over twice that of individuals who do not abuse opioids. Among those whose opioid habit is severe enough to justify a SUD diagnosis, 23% seriously contemplate suicide. The British Medical Journal published research revealing that any person who has ever attempted suicide is at-risk for the remainder of their life. More than 20 years after a previous attempt, the suicide risk remains two-and-a-half times greater than people without such a history. Psychiatrist Dr. Gary R. Jenkins, with London’s East Ham Memorial Hospital, says, “This confirms something we know about suicide, that the best predictor is a previous attempt…This paper proves what we have thought clinically — a previous attempt is a predictive factor even if it is more than two decades after the first act.”
Warning Signs of Suicide
“When people are suicidal, their thinking is paralyzed, their options appear spare or nonexistent, their mood is despairing, and hopelessness permeates their entire mental domain.”~ Kay Redfield Jamison, Night Falls Fast: Understanding SuicideIf someone exhibits several of the following suicide warning signs, they need immediate psychiatric help:
- Appearing depressed or sad most of the time
- Frequently writing or talking about death or suicide
- Social withdrawal or isolation from family and friends
- Feelings of helplessness or hopelessness
- Rage or angry outbursts
- Feelings of being “trapped”, with no other way out
- Suffering overwhelming stress
- Major unwanted life changes
- Loss of a loved one
- Dramatic mood swings
- Substance abuse
- Personality changes
- Out-of-character impulsiveness or recklessness
- Abandonment of once-enjoyed interests and hobbies
- Poor OR excessive appetite
- Lack of sleep OR excessive sleeping
- Poor work or academic performance
- Overwhelming guilt or shame
- Getting rid of personal possessions
- Suddenly writing a will
- Making statements like, “When I’m gone…”
It is important to understand that while not everyone who kills themselves shows any warning sign… but 3 out of 4 DO.If you feel that someone is in immediate danger of self-harm, CALL 911.For anyone considering such a desperate act, people are available to talk to and to listen, day or night, every day of the week, at the National Suicide Prevention Lifeline.
The Dangers of Smiling Depression
“So, for me, grief, trauma, pain, loss became an issue that I hid away. Like an anorexic person hiding food, like an alcohol-dependent person hiding their drinks, I found a hiding place for my pain.”~ Jeannette Fagan,Within The Madness That is GriefUnfortunately, the warning signs of depression are not always obvious from the outside. Many people live in a secret crisis. This is especially true for those who appear “successful”. They may fool other people—and even themselves—that they are fine, when in reality, they are struggling.This is known as“Smiling Depression”. With this manifestation, sufferers may be outwardly happy and well-adjusted. They usually work full-time, are popular and active socially, and have caring family and friends. By most measures, they appear to be successful.But on the inside, they are hurting—plagued by overwhelming anxiety, despair, self-doubt, and loneliness. They often have a drug or drinking problem that they keep well-hidden from others, thereby preserving their carefully-maintained public image.For them, suicidal thoughts are a real concern. In fact, people with this atypical depression are often more likely to harm themselves than individuals with more common variety. While people with severe depression may frequently think about taking their own life, they often lack the will and the energy to act on those thoughts. But people with smiling depression DO have the ability to plan and DO have the energy follow through.In their mind, it comes as a relief, because they no longer have to go through the motions or put forth the effort to pretend that everything is perfect.
Depression during Withdrawal and Recovery
“Even if you can stay in recovery from your addictions, as long as you hold on to the fear, anger, and grief, there’s a good chance you’ll either pick up another addiction or return to a previous one.”~ Barb Rogers, Addiction & Grief: Letting Go of Fear, Anger, and AddictionFor people with severe clinical depression, even sobriety and recovery can be dangerous. When a person who is severely dependent on or addicted to drugs or alcohol tries to quit, they quickly experience harshly unpleasant withdrawal symptoms. This includes a debilitating depression that can be so severe as to completely disrupt their newly-sober life. In fact, withdrawal is often so physically and emotionally painful that the person relapses and resumes use, just so they can find a measure of relief.And while the worst withdrawal symptoms usually subside within a matter of a few days or weeks, Post-Acute Withdrawal Syndrome is another matter. Depending upon the person’s history of substance abuse, the severity, length of their addiction, and the specific substance, the symptoms of PAWS can linger or flare up for months or even years after cessation of use.Withdrawal-related depression is worst in someone who is already prone to illness.But there is good news. With enough time, personal support, and when appropriate, the help of certain medications, the brain’s chemistry will eventually restore itself and return to normal balance. In other words, withdrawal-related depression is TEMPORARY.Persistent depression and other withdrawal symptoms show the importance of long-term aftercare in terms of achieving lasting sobriety and successful recovery.
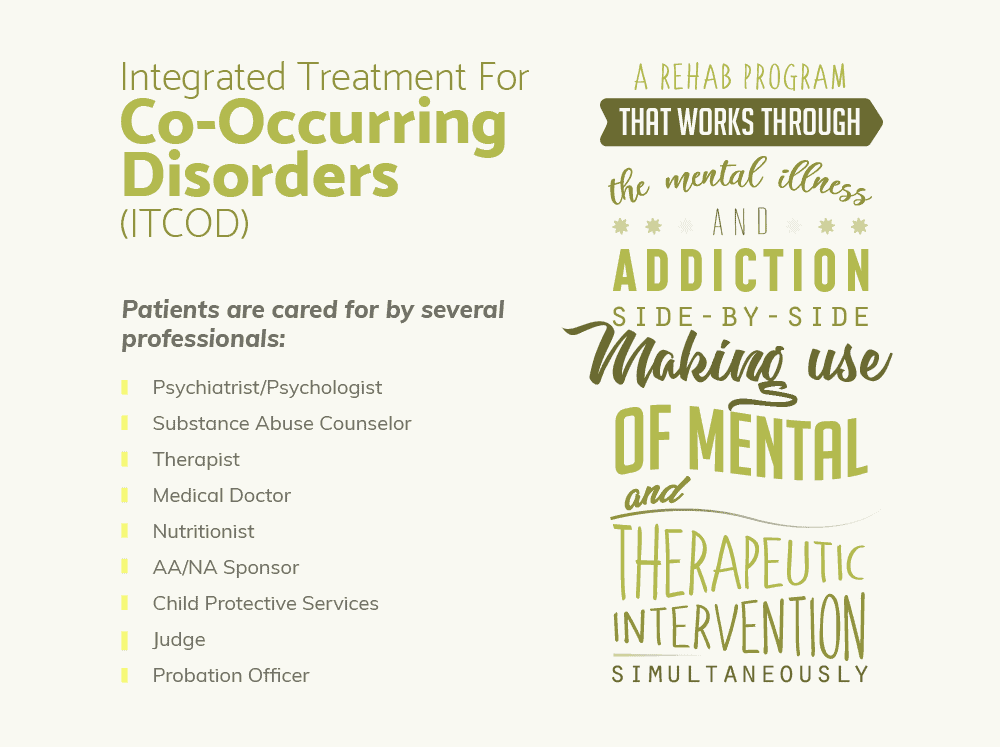
Help for a Dual Diagnosis
“…each disorder exacerbates the other and also predisposes to relapse in the other. At times, the symptoms can overlap or even mask each other, making diagnosis and treatment all the more difficult.”~ Robert B. Pereia, Faces of Dual Diagnosis: A Canadian PerspectiveWhen addiction and mental illness co-occur, successful recovery gets complicated. Without the right kind of treatment plan, the specific difficulties associated with each disorder undermine any progress.The Substance Abuse and Mental Health Services Administration only recommends one course of action for dual diagnosis – Integrated Treatment for Co-Occurring Disorders.This treatment model was specifically developed for people with SUD and co-occurring mental illnesses. With an integrated treatment plan, patients are evaluated and treated by a single cooperative team of professionals, rather than by different providers at separate facilities.There are several advantages to this approach.FIRST, when counselors, addiction specialists, mental health professionals, and medical personnel are able to work together under the umbrella of shared treatment philosophy, there is a much better chance of a positive outcome.SECOND, this kind of teamwork, cooperation, and communication means that any issues that arise can be dealt with that much faster and addressed by all parties. It also makes it easier for the team to make any needed adjustments to the treatment plan.THIRD, it allows providers to treat BOTH disorders as the primary condition. This is important because since both addiction and depression can each worsen the other, both must be treated at the same time. Any other approach that treats them separately or sequentially could lead to setbacks or even relapse.But despite the endorsement from the SAMHSA, most rehab programs do not offer ITCOD. Primarily, this is because this treatment approach requires a significant commitment on the part of the rehab, in terms of time, resources, personnel, and training.For example, the “Gold Standard” of addiction care is Medication-Assisted Treatment that combines behavioral counseling with FDA-approved medications that reduce drug cravings and alleviate withdrawal symptoms. But some of these medications require prescribers to receive extensive additional training and obtain a special license before they are allowed to give them to patients. As a result, just 3% of doctors in this country are able to prescribe such effective anti-craving medications as Vivitrol, the once-monthly injection used to combat opioid addiction.As an unfortunate result, only about 12% of people with a dual diagnosis ever receive the proper treatment for both their addiction and their mental disorder.
The Bottom Line—What Does This Mean to YOU?
The most important takeaway is how closely-related addictive and psychological disorders truly are. If you are struggling with either, the best thing you can do to support your successful recovery is to get professionally evaluated for the possibility that you might have both.The next thing to keep in mind is how serious a dual diagnosis is. Depression and SUD are each potentially-fatal health conditions on their own, and the risks are magnified when they present simultaneously.Also, successful recovery is best served when the treatments of both disorders are of equal importance. This is the most effective way to support sobriety, promote good mental health, and prevent relapse.Next, such a complicated dual diagnosis requires a treatment plan that is both integrated and comprehensive. After a thorough evaluation, the services should be tailored to you as an individual, using an approach that addresses each disorder on multiple levels.Finally, not all rehabs are created equal. This means that to find a program that is qualified to treat your dual diagnosis, you may have to do a little homework and legwork. But by making the effort asking the right questions, you will put yourself in the best possible position to safely and successfully regain both your sobriety and your mental health.
What Did you Think About This Blog?
Give it a Rating!